Gene Therapy: Revamping Viruses from Fiends to Friends
Dec 21, 2020 | 3 min read
Dec 21, 2020 | 3 min read
Viruses have been considered the bane of human existence ever since the first one - Tobacco Mosaic Virus, was identified by Dmitri Ivanovsky back in 1892. Whether it be causing fatal human diseases like Ebola and AIDS or bringing about
destruction to millions of acres of economically vital crops, they have proven to be a thorn in our side time and again. But nearly 30 years ago, on September 14, 1990, an attempt was made to show viruses in a new light.
Ashanthi was a four-year-old girl suffering from Severe Combined Immunodeficiency (SCID). This meant that she had nearly zero immunity against most of the existing diseases, forcing her to wear protective gear that isolated her completely
from the external environment. Such patients were called bubble babies, and they hardly had any choice other than to live life this way. In a stroke of genius, W. French Anderson and his colleagues at NIH conducted one of the first approved
gene therapy procedures on Ashanthi, who showed rapid improvements in her WBC count over a span of just two years.
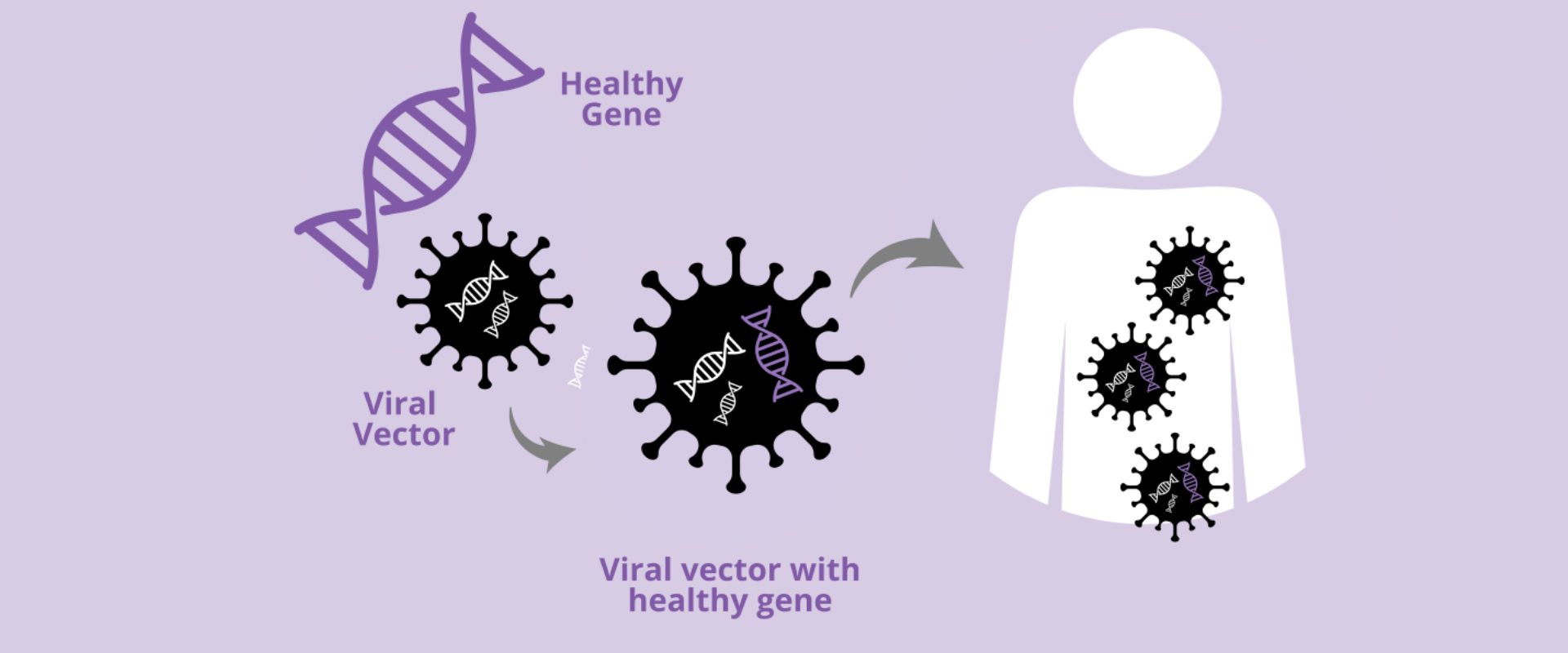
The way Gene Therapy works is that a new recombinant DNA is inserted into the genome of the patient, effectively replacing or taking over the function of the gene that was responsible for the patient’s initial condition. For the success
of such a method, there are a few conditions that must be met. The vector must be immunologically inert, it must prevent the genetic material from being degraded and it must replace the gene at the specific target site. Viruses have gone
through millions of years of evolution to perfect this art of entering a host cell and integrating their DNA into the cell’s genome, making them the perfect candidate for the procedure. The self-replicating capability of these viruses is
smothered while their genome integration ability is kept intact to make sure that they are safe enough to be injected into the human body. Gene therapy has developed by leaps and bounds with retroviruses and adenoviruses being the ones
that have most commonly been manipulated to submit to our will.
A lot of research has also gone into developing non-viral vectors for gene therapy. Natural polymers such as Chitosan as well as synthetic ones like Poly Ethylene Glycol (PEG) are being used for the same. The electrostatic interactions
between such cationic polymers and negatively charged DNA facilitate the process of gene integration in this case.
But there still remain many ethical issues regarding gene therapy, mostly the viral route. The major concerns are that replication-competent viruses might accidentally be produced when the vectors are being prepared or that the vectors
that are inserted may be used by a preexisting endogenous retrovirus in the human genome as a means of remobilization and packaging of their genetic material. In 1999, Jesse Gelsinger, an 18-year-old diagnosed with Ornithine Transcarbamylase
Deficiency Syndrome (OTCD), became the first victim of a failed gene therapy attempt when his body reacted violently to a batch of adenoviruses entering his liver. Such incidents serve as a harsh reminder that while humans have come a long way
in probing and unraveling the secrets of life, they may never truly be able to play God.

Figure 1. David Vetter a bubble baby from Texas. He can be seen wearing a NASA designed spacesuit that separates him from the external environemnt. He was born with Severe Combined Immunodeficiency disease (SCID) in 1971.
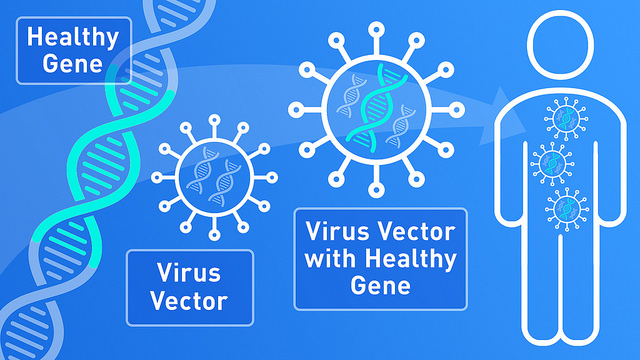
Figure 2. This is a schematic for the procedure of Gene Therapy. Here, we can see the importance of a viral vector in this process.